Case Report
Large L5/ S1 Disc Protrusion Referral for Treatment and Management using Cox® Flexion-Distraction Therapy.
AUTHOR: Dr Danica Newbold (B.HSci (Chiro), M.ClinChiro, Ad. Dip Myo) Malvern Chiropractic and Melbourne Spine Clinic (Melbourne, Australia).
HISTORY: Ms N presented to Malvern Chiropractic Clinic and Melbourne Spine Clinic (Melbourne, Australia) on 11th June 2020 with a large L5/S1 disc protrusion and right-sided radiculopathy. She is a 40-year-old woman, who works full time as an Architect. Ms N was referred to our clinic by her former Chiropractor, who reached out on social media looking for a Practitioner who utilised Cox® Flexion-Distraction therapy.
On initial presentation, Ms N described eight (8) months of right-sided lower back pain and right-sided sciatica, involving mild to moderate pain in the gluteal region, posterior leg, calf and plantar surface of the right foot. There was some mild transient paraesthesia and anaesthesia in the right calf and foot, and she described her pain as a “deep aching sensation with intermittent heaviness” in the right leg and foot. Her initial VAS score was marked as 6/10. Ms N noted that her pain increased when sitting or standing, even for short periods, which proved disruptive to her work life. She found mild relief from some light exercise, such as walking and stretching, as well as some relief from her previous Chiropractor, who referred Ms N to our clinic. Ms N’s previous Chiropractor, who worked with her for the preceding two months on managing her pain, was a low-force practitioner who used Sacro-Occipital Technique (SOT), Activator® and soft tissue therapies. Ms N also saw a Naturopath who prescribed her several supplements, including Magnesium, Multi-Vitamin, Vitamin D + K2, Vitamin B Complex, a Probiotic, and a Naturopathic supplement for hormone balance adrenal function.
Ms N was referred initially for plain film x-rays with her previous Chiropractor and then referred for a Lumbar Spine MRI study approximately six (6) weeks later. Both reports and images were presented and reviewed at her initial consultation in our clinic.
EXAMINATION FINDINGS:
An initial examination performed on 11th June 2020 revealed the following:
Range of Motion (ROM):
Lumbopelvic ROM (active) was mild to moderately reduced in all planes, most notably in right lateral flexion and rotation, with mild pain at the end range.
Palpation:
Hypertonic and tender muscles of the lumbopelvic region, including the lumbar Erector Spinae (ES), Gluteal muscles and Piriformis (R>L). Spinal joint tenderness and rigidity were noted over the right L5/S1 and right sacroiliac region.
Neurological and Orthopaedics:
Reflexes were tested and noted as:
- Reduced (+1) S1 (Achilles) reflex on the left and absent on the right.
- All other lower limb reflexes were unremarkable.
Myotomal screening revealed weakness in the right lower limb without pain reproduction. The following values were noted on initial examination:
- Extensor Hallicus Longus right 4/5,
- Gluteus Maximus bilaterally 4/5,
- Piriformis right 4/5,
- Hamstring right 4/5.
Orthopedics testing returned positive results for:
- seated SLR at 45 degrees,
- Slump test,
- Ely (mild) and Mennells (mild).
Also noted was a mild right short leg indicative of a mild pelvic distortion pattern.
IMAGING:
Full spine plain film x-rays and a lumbar spine MRI were performed before her initial presentation to our clinic. Spinal x-rays were conducted on 6th March 2020, and the radiologists report identified the following:
- Minimal straightening of cervical lordosis with subtle anterolisthesis at C4/5. Degenerative uncovertebral and facet changes were also noted in this region—minimal biconcave thoracolumbar scoliosis with a measured Cobb angle up to 5mm. Anatomical AP alignment is maintained.
- Minimal facet and endplate degenerative changes were noted throughout the lumbar spine.
With little change in Ms N’s condition, her previous Chiropractor referred her for a lumbar MRI scan approximately seven (7) weeks later. Studies performed on 23rd April 2020 identified the following:
- There are very minor generalised disc bulges from T11/12 to L3/4 with mild generalised disc bulge at L4/5.
- Very mild bilateral lumbar facet joint arthropathy.
- Large right paracentral/ subarticular disc protrusion measuring 11mm (AP), displacing thecal sac to the centre and impingement of right S1 nerve root with displacement of the right S2 nerve root.
- Mild subchondral sclerosis of bilateral sacroiliac joints.
- Atrophy of lower bilateral lumbar erector spinae muscles.
Please refer to the images below (Fig 1 and 2).


TREATMENT AND RESULTS:
Ms N was treated using Cox® Flexion-Distraction and Spinal Decompression Therapy over several sessions focusing on the right L5/S1 discal compartment decompressing the right S1 and S2 nerve root irritation.
At session one (1), the patient was having a particularly uncomfortable day with increased sciatic pain and moderately restricted ranges of motion. Ms N could not sit for longer than 30-60 seconds and found walking around the treatment room beneficial. Following on from tolerance testing before therapy application, the patient could only manage to receive long y-axis distraction, minimal Protocol 1 applications to the lumbar spine (‘5-4-3 Method” – 5 repetitions, over 4 seconds in 3 groups) and soft tissue therapies using an electric percussion massage tool, to the lumbopelvic region. The patient was advised to conduct self-care at home post-treatment consisting of rest and cryotherapy (cold/ ice packs)- 10 minutes of cold/ice pack use every hour for 24-48 hours. She was also provided with a lumbosacral support belt to wear.
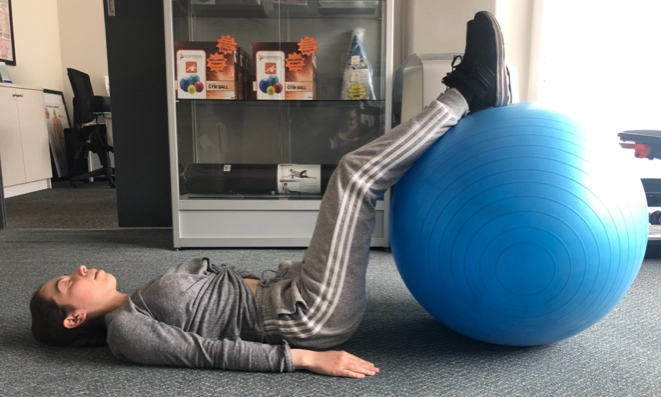
Ms N had her follow up appointment two (2) days later on 13th June 2020, with decreased pain post initial treatment. Ms N was able to sit and walk better and longer and noted that she is still feeling sciatic pain in the right gluteal region and tingles in the right foot. Protocol II (2) Flexion-Distraction Therapy (long y-axis traction, flexion, lateral flexion and coupling movements by ten repetitions at approximately 50% intensity) was performed to the lumbar spine with good tolerance. Treatment included targeted soft tissue therapies to the lumbopelvic region, and the patient was prescribed very gentle low-impact spinal stretch exercises using an inflatable exercise/ gym ball. Please see the images below of specific stretches (Fig 3 and 4).

By session three (3), on 16th June 2020, Ms N had no distinct or noticeable pain in her lower back. She still felt a slight tingle in the right foot and mild tightness in the right glute. VAS score was taken and noted at 2/10 (greater than 50% improvement). The Range of Motion had improved, and she could perform them without pain. Flexion-Distraction Protocol II (2) (long y-axis traction, flexion, lateral flexion and coupling movements) was increased to full intensity at this session and continued throughout the treatment plan, increasing the movements within the patients’ tolerance with each subsequent session.
At session four (4) on 18th June 2020, Ms N noted a VAS score of 1-2/10. Her pain quality had decreased in both frequency and intensity, as had the paraesthesia in the right foot. She particularly noted that she did not feel any tingling in the foot in the morning anymore. At this session, we introduced the ankle cuffs to the patient’s treatment plan with good acceptance. Ms N was advised to continue her prescribed stretches and increase her walking within her tolerance.
In session six (6), Ms N noted that she would attempt skiing on an upcoming weekend getaway. The paraesthesia in her right foot only lasts 5-10 mins on any given day, and she had no gluteal pain or lower back pain. She had begun increasing her exercise routines with her personal trainer, expanded her weight-training practices, and did more dynamic exercises. We continued to apply Cox® Flexion-Distraction Protocol II (2) to decompress the L5/S1 spinal disc level. At this session, Ms N was prescribed core and trunk muscle activation exercises. Ms N returned from her ski weekend feeling good. She did not experience any increase in pain, discomfort, muscle tightness or paraesthesia. We then discussed decreasing the frequency of her appointments and scheduled our next appointment for one (1) week later.
By mid-August 2020, Ms N reported no low back pain, sciatica or paraesthesia on the right side. We began including Chiropractic treatments for multiple spinal regions (thoracic and cervical) and some low-force Activator®-style adjustments to the upper extremities to combat postural spinal joint strain and upper limb biomechanical discomfort. Ms N finds in her line of work (Architecture) that the long hours spent at a desk, computer, or hunched over large drafting tables to be problematic for her spinal health and that specific exercises (i.e., handstands, push-ups, and free-weight training) with her personal trainer can cause the wrists and elbows to become stiff, fixated and uncomfortable. Ms N implemented my advice to change her desk ergonomics early on – this included using a Sit-Stand desk, alternating a desk chair with an exercise fitness/ gym ball and taking regular breaks (every one to two hours) to perform spinal flexibility stretches.
PROGNOSIS:
Ms N’s progress through the treatment program was excellent, and she was able to return to regular ADLs quite quickly. She attended her sessions as indicated and, by appointment number 14 (10 weeks post initial consultation), shifted to a maintenance style program (monthly sessions).
Re-evaluation of the initial examination findings demonstrated an overall improvement in ROM to complete and pain-free movements. Orthopaedic and neurological testing indicated inconsequential compromise at the L5/S1 discal compartment level and S1/S2 nerve root level.
Ms N continues to attend regular appointments in our clinic and maintains a 90-100% improvement in overall pain and discomfort. She continues to receive Cox® Flexion-Distraction Protocol II (2) to her lumbar spine, targeted soft tissue therapies manual diversified spinal manipulation to the thoracic spine and low-force Activator-style adjustments of the upper extremities.
Plans for update MRI studies to re-evaluate Ms N’s significant L5/S1 disc bulge are scheduled for six (6) months’ time with the focus on re-assessing the size and neurological compression of the previously imaged discal compartment.
CONCLUSION:
Ms N currently does not display any of her original signs and symptoms and receives monthly treatment to maintain her pain-free lifestyle. More recently, Ms N had a flare-up of right-sided upper thoracic pain, for which we increased her treatment program to best suit, and she has now returned to her maintenance style treatment program.
I remained in contact with Ms N’s former Chiropractor privately via social media in relation to her condition and her progress through the treatment plan. She appreciated the update and was pleased to know that Ms N was well taken care of.
Cox® Flexion-Distraction and Spinal Decompression Therapy was the appropriate treatment method for this patient’s condition, as demonstrated by the successful subjective and objective outcomes achieved. This case report proves the positive outcomes for the patient-focused cooperation within the Chiropractic profession in Australia and, I look forward to helping more patients and healthcare professionals understand the benefits of Cox® Flexion-Distraction and Spinal Decompression Technic.
REFERENCES:
- Cox JM, Feller J, Cox J. Distraction Chiropractic Adjusting: Clinical Application and Outcomes of 1000 cases. (1996).
- Low Back Pain: Mechanisms, Diagnosis and Treatment. James M Cox. 7th Ed. Lippincott, Williams & Wilkins. 2011.
- Gudavalli MR: Estimation of dimensional changes in the lumbar intervertebral foramen of lumbar spine during flexion distraction procedure. Proceedings of the 1994 International Conference on Spinal Manipulation, June 10‐11, 1994, Palm Springs, CA, pp 81.
- Gudavalli MR, Cox JM, Baker JA, Cramer GD, Patwardhan AG: Intervertebral Disc Pressure Changes During a Chiropractic Procedure. Proceedings of Bioengineering Conference, Phoenix, 1997



