Case Report
Complex multi-segmental spinal pain in 48-year-old male patient post-surgery with tri-level spinal fusion and double synthetic disc replacement managed with Cox® Flexion-Distraction Technic.
AUTHOR:Dr Danica Newbold (B.HSci (Chiro), M.ClinChiro, Ad. Dip Myo) Malvern Chiropractic and Melbourne Spine Clinic (Melbourne, Australia).
PRESENTER: Dr Joel Dixon (B. App.Sc (Chiro), J.P., Certified Cox® Flexion-Distraction Instructor); Malvern Chiropractic and Melbourne Spine Clinics (Melbourne, Australia). February 2023 Cox® Technic Honors Course- Maui, Hawaii (USA).
HISTORY
Mr H, a 48-year-old male IT worker, presented to Malvern Chiropractic Clinic and Melbourne Spine Clinic (Melbourne, Australia) on the 24th of April 2022 with a long and complex history of low back pain and dysfunction associated with a traumatic windsurfing injury sustained in 1999.
Unfortunately, Mr H was thrown from his windsurfing board in the air approximately 8-10 meters (25-30 feet approximately) and crash-landed in the ocean with significant force. He immediately felt low back pain, but it was not until several days later that he experienced any radicular pains. Predominantly left-sided, his leg pains progressively worsened over a short period (the patient could not recall precisely what time frame this was) before investigations were initiated.
In December 1999, Mr H underwent his first lumbar spine MRI scan, which identified a moderate left-sided disc extrusion/sequestration at L4/5, diffuse left-sided disc extrusion at L5/S1 and mild disc bulge at L3/4 with annular eruption.
Mr H had undergone many scans over the history of his spinal pain condition (please see Imaging further on for more details), and after trying many conservative and prescriptive options to find relief for his pain, Mr H underwent numerous intraspinal injections before undertaking a three-level Percutaneous Disc Decompression (Nucleoplasty) procedure at L3/4, L4/5 and L5/S1 in January 2005. Unfortunately, this did not provide the outcome that the patient and pain specialist had hoped for.
In May 2005, Mr H underwent his first open surgical procedure – Two synthetic disc replacements at L3/4 and L4/5 with an L5/S1 fusion. This surgery was deemed successful as Mr H was no longer experiencing left-sided radicular pain. Mr H successfully completed his post-surgery rehabilitation program and slowly began returning to some regular activities of daily living.
By March 2006, Mr H was still experiencing significant lower back pain and underwent a revision surgical procedure to remove the inserted hardware for the L5/S1 fusion. According to Mr H’s memory of the events, – an unsurprising common occurrence, according to the orthopedic surgeon. By this point, a “natural” fusion of L5/S1 had stabilised this level from ectopic bone growth and did not require further surgical intervention. Based on Mr H’s recollections, the surgeon may also have repaired a small avulsion of the muscles attached to the iliac crest (possibly iliocostalis lumborum) during this same procedure.
Mr H was still experiencing diffuse pain in the right lower back and underwent a right L5 transforaminal nerve root injection in July 2006 to see if this would reduce his discomfort. In 2008, Mr H was still in pain and seeking different conservative interventions, including Chiropractic, Osteopathy, Physiotherapy, Massage, Exercise Rehabilitation, Acupuncture and Feldenkrais, with limited success. Continuing to progress and persevere, Mr H continued to do what he could to relieve his condition.
Mr H was quite an active person in the years before COVID-19. He regularly rode his bike to and from work (approximately 10-15km each way), sailed on his boat, regularly completed household activities at his small farm and swam either in the ocean or pools. However, since the COVID-19 lockdowns in Australia from 2020 to 2022, Mr H’s lifestyle has become more sedentary, and as a result, he noticed his peak fitness levels decrease and back pain return.
Once Mr H had presented to Malvern Chiropractic Clinic and Melbourne Spine Clinic, we began applying the knowledge and understanding of many years of study to alleviate Mr H’s spinal discomfort. Mr H was thoroughly examined and evaluated before commencing therapy, and he was referred again for updated imaging (MRI and CT) to establish what was currently going on with his spine.
IMAGING
Mr H has had multiple imaging studies performed in his complex history. His first image investigation was a lumbar spine MRI performed on the 5th of December 1999 after the initial mechanism of injury (MoI), which concluded:
- “There is a moderate left paramedian disc extrusion at the L4/5 level with extruded and possibly sequestered disc material, compressing the left L5 nerve root. Left diffuse posterior disc extrusion at L5/S1 and a mild disc bulge at L3/4 that contains a region of T2 hyperintensity consistent with annular disruption. Neither contacts neural structures.”

Approximately six (6) months later, in June 2000, repeat Lumbar MRI scans were performed as Mr H was still experiencing significant pain and left-sided sciatica. It deduced:
- “L4/5 mild posterior broad-based disc bulge with moderate superimposed central disc extrusion more pronounced on the left side than the right, which compresses the left L5 nerve root within the lateral recess. In addition, there is a sequestered disc fragment more inferior to this situated anterior to the left side of the thecal sac. This also contacts the left L5 nerve root within the lateral recess.
- L3/4 mild posterior broad-based disc bulge with superimposed small central disc protrusion, which does not displace or compress neural structures
- L5/S1 mild posterior broad-based disc bulge which contacts the anterior aspect of the S1 nerve root bilaterally as they exit the thecal sac.”
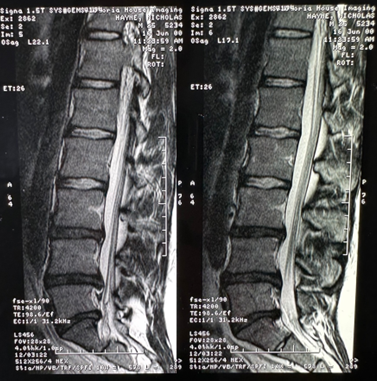
Additionally, a week later, a Lumbar spine CT scan was also performed:
- “Moderate to large left paracentral L4/5 disc protrusion. Mild central posterior disc protrusion at L3/4. Mild right paracentral disc protrusion at L5/S1.”
By October 2002, Mr H had not experienced much relief in the pain and symptoms (post interventions). Still experiencing chronic Low Back Pain (LBP), another Lumbar spine MRI scan was performed.
- ” Frank desiccation of the L3/4, L4/5 and L5/S1 discs set on a background of a constitutionally narrow canal. A moderate central disc protrusion is noted at L3/4. There is extensive annular tearing of the L5/S1 disc with bulging towards the right side and displacement of the right S1 nerve root.”
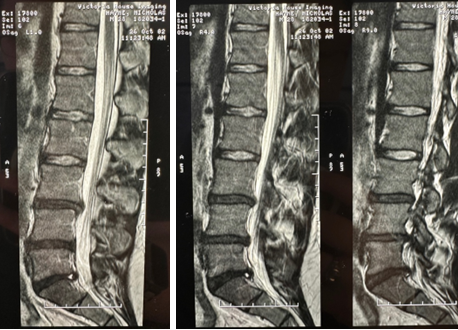
Further along and several different interventions later, Mr H was still experiencing chronic pain. In July 2004, another MRI scan was performed.
- “Desiccation of the lower three intervertebral discs. Moderate-sized central disc protrusion at L3/4 with a radial fissure and abutment of the exiting L4 nerve roots. Central to left-sided disc protrusion at L4/5 without any neural contact, moderate-sized central to right-sided protrusion at L5/S1 deforming the right S1 nerve root.”

It was some time before any further imaging was performed. In March 2008, a lumbar spine MRI scan was conducted as Mr H was experiencing worsening right low back pain (LBP). It concluded:
- “Small central annular tear without significant disc bulge at L2/3. The central canal remains capacious, and exiting nerve roots are unimpeded.”
- “Within the paraspinal musculature from the L4-5 level inferiorly, there is moderate extensive T2 high signal, without a focal fluid collection and reasonable preservation of fat planes on T1 weighted imaging. Less avid but similar changes are seen in the paraspinal musculature on the left, immediately superior to the iliac crest. This appearance is most likely related to post-surgical scarring and granulation tissue.”
As part of the investigative process in our clinic, Mr H was referred for updated imaging. Initially, an updated Lumbar spine MRI scan was performed on the 1st of June 2022. It reported the following:
- ” Mild central canal stenosis due to mild broad-based disc bulging with endplate spurring. This is increased in severity when compared with previous MRI studies.”
- “Unfortunately, due to previous surgery, there is poor detail from L3/4 – L5/S1 due to bloom artifact effect, which obscures details.”
The radiologist did suggest that a CT scan of the lumbar spine could be performed with metal artifact reduction (SEMAR) to enable better visualisation of these levels.
On the 27th of July 2022, a CT scan of the lumbar spine was performed. It identified the previously obscured spinal levels from the MRI study. The following was noted in the report:
- “No acute disc protrusions. L3/4, L4/5 and L5/S1 fusions with disc replacement devices in situ. Mild lucency of the posterior margins of the L3/4 disc replacement device suggests focal loosening”.
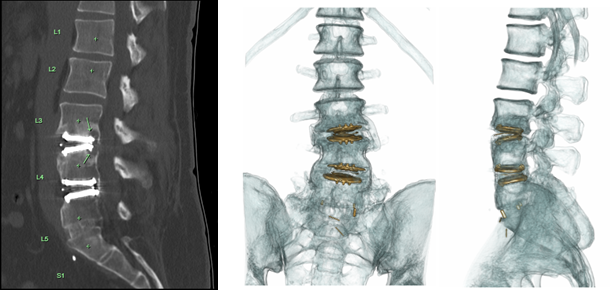
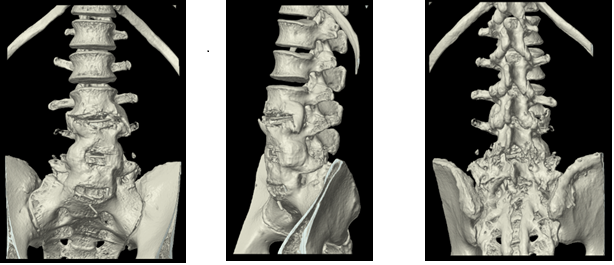
As a result of this information about the L3/4 artificial disc, a referral to a local Orthopedic Surgeon was advised to the patient for further investigation.
SURGICAL INTERVENTION: Based on years of chronic pain and suffering he had experienced and numerous unsuccessful interventional procedures, Mr H sought the expertise of an Orthopedic Surgeon in Victoria (Australia). At the time, very few spinal surgeons were performing such interventions, so Mr H had to travel 3-4 hours north of Melbourne (Australia) to seek the assistance of this particular surgeon.
In May 2005, after his examination and review of radiological findings, it was determined that a tri-level procedure involving Synthetic Disc Replacements at L3/4 and L4/5 and an L5/S1 fusion would be able to provide Mr H with better long-term outcomes for his pain and neurological symptoms (see post-op x-rays below). Mr H completed his in-hospital post-surgical rehabilitation and was prescribed continuing exercises to aid his recovery by the rehabilitation Physiotherapist.

While this initially relieved Mr H’s low back pain and left-sided peripheral neuropathy, Mr H began feeling increasing lower back pain return. In March 2006, Mr H underwent a second surgical procedure with the same Orthopedic Surgeon. The surgeon removed the screws for the L5/S1 spinal fusion during this second surgical intervention. Significant ectopic bone had grown around this spinal level, and further stabilisation of this fusion was not needed.
EXAMINATION FINDINGS:The following was noted on initial examination at Malvern Chiropractic Clinic and Melbourne Spine Clinic.
- Mr H described his right-sided low back pain and hip pain as a constant aching tightness with bilateral hamstring tightness (R>L), and pulling into the right flank, hip/posterolateral gluteal region.
- The initial VAS score was noted as 6/10.
- As his condition had been aggravated over the last couple of years due to COVID-19 restrictions and lockdowns, Mr H took over-the-counter (OTC) analgesics and ibuprofen to manage his pain levels as needed.
Range of Motion (ROM):Lumbar range of motion (ROM) was severely adapted to the altered biomechanics in his lumbar spine due to spinal dysfunction and fixations from L3-S1. Mr H’s ROM was moderately within normal limits with some mild restrictions in Lateral Flexion and Rotation of the torso. AROM at L1/2 and L2/3 demonstrated mild restrictions in lateral flexion (15o) and rotation (10o). Lumbar flexion was unrestricted – was able to toe touch.
Palpation:Complete rigidity and fixation of L3-S1 was confirmed on palpation without tenderness or discomfort. Mild tenderness and rigidity were noted at the L1-2 spinal levels (R>L). Hypertonicity of the lumbar erector spinae muscles (R>L), right quadratus lumborum and bilateral gluteal group and hamstrings (R>L) were also noted.
Neurological and Orthopaedics:Straight leg raise (SLR) was negative for neurological compromise; however, given the hypertonicity of the bilateral hamstrings, Mr H experienced intense muscle cramping of the bilateral hamstrings on testing. All other orthopedic tests were negative. Neurologic examination demonstrated decreased bilateral patella reflexes (+1) and left achilles reflexes (+1). The right Achilles reflex was absent (0). Decreased strength was noted in the left extensor hallicis longus (EHL) and left tibialis anterior (4/5). A mildly right-shortened leg by approximately 3-4 mm was also indicative of a mild pelvic distortion pattern.
TREATMENT AND OUTCOMES:Since his initial presentation, Mr H has received Cox® Flexion-Distraction and Spinal Decompression Therapy focusing on the upper lumbar spinal levels (L1/2 and L2/3) and synchrony and symmetry of the sacro-iliac joints (SIJ). Treatment goals:
- Reduce excessive strain on the discal compartments and apophyseal joints at L1/2 and L2/3 associated with the lumbar spinal fusions below and retard degradation patterns in 48 yro post-surgical male.
- Improve Active/Passive ROM throughout the unfused spinal levels.
- Reduce SIJ asymmetry.
- Improve bilateral spinal muscle symmetry and flexibility.
At Mr H’s first (1) session, after his thorough examination and review of the large consortium of scans and reports regarding his long, complex spinal pain history, Mr H was advised on all aspects of the Cox® Technic, and treatment began. Cox Flexion-Distraction Protocol I (1) (“5-4-3 Method” – 5 repetitions, over 4 seconds in groups of 3) was implemented to the L1/2 and L2/3 spinal compartments following tolerance testing with good tolerance. The patient was advised to conduct self-care at home post-treatment consisting of relative rest (short periods of movement/ walking encouraged) and cryotherapy (cold/ ice packs)- 10 minutes of cold/ice pack use every hour for 24-48 hours.
Mr H had a follow-up consultation five (5) days later, on the 5th of May 2022, with no increased pain or discomfort. He reported experiencing slight relief in the generalised stiffness. We have continued to decompress the L1/2 and L2/3 compartments and implemented Cox® Flexion-Distraction Protocol II (2) (long y-axis traction, flexion, lateral flexion by ten repetitions at approximately 50% intensity) with good tolerance.
By session three (3) on the 9th of May 2022, Mr H was still experiencing similar tightness but had no increased pain or discomfort and reported not feeling as stiff. Flexion-Distraction Protocol II (2) was continued and increased to full intensity throughout the treatment plan, increasing the movements within the patients’ tolerance with each subsequent session.
Given the length of time, it was decided that a new MRI scan would be requested since updated scans had long been performed before presenting to our clinic. An MRI was conducted and reported on the 1st of June 2022 (see conclusion above). Unfortunately, metallic blooming from the artificial disc replacements obscured the detail required to examine the L3/4 to L5/S1 spinal levels. It was suggested that a CT scan of the lumbar spine with metal artifact reduction (SEMAR) might better visualise the lower lumbar spine.
At session six (6) on the 7th of June 2022, Mr H reported a VAS score of 4/10 and noted getting a couple of days of relief in regular symptom presentation. Unfortunately, Mr H is still very inactive and has not begun any forms of exercise to aid in his recovery. Mr H was prescribed basic lumbar spine stretches using an Exercise Ball as a jumping-off point for his rehabilitation. He was also encouraged to get back into walking and swimming.
In session eight (8) on the 21st of June 2022, Mr H had a long weekend prior of gardening at his small farm. Typically, this would aggravate Mr H’s lower back pain and intense muscle tightness; however, he finally felt pressure reduction in his lower back. Unfortunately, by the follow-up session one week later, after another round of gardening, Mr H experienced right-sided lower back tightness referring to the right hip/ flank area. This increased his VAS score to 5/10.
On the 2nd of August 2022, Mr H completed the CT scan and presented the findings. Stenotic compression of the right-sided L4/5 neurological compartment and possible instability due to focal loosening of the L3/4 artificial disc. It was advised that Mr H seek the opinion of an orthopaedic surgeon to assess the instability of the L3/4 synthetic disc for any potential neurological compromise.
By appointment 16 on the 8th of August 2022, Mr H reported an updated VAS score of 2-3/10 (50% improvement). Subjectively he reported improvement in the overall tension and stiffness but still noticed the pulling feeling into the right hip/ flank area; however, he did experience glimpses of release in this area. Exercise is still intermittent at this point.
September came, and Mr H began bike riding more often, and other than some tightness in the legs and hamstrings (Delayed Onset Muscle Soreness-DOMS), he did not report any increase in low back pain or right hip./ flank pain. We continued Cox® Flexion-Distraction spinal decompression Protocol II at full intensity without pain or discomfort.
In early October 2022, Mr H had his consultation with the Orthopaedic Surgeon. We received his correspondence letter briefly detailing his discussion with Mr H. He explained that he was not overly concerned with the focal erosion around the L3/4 disc replacement and believed it to be relatively stable, and the likelihood of requiring any further surgery on his lumbar spine is minimal.
Mr H continued to ride his bike for extended periods and could now ride for approximately 1 to 1.5 hours without issues or pain. Depending on the level or type of activity, Mr H occasionally experienced muscle spasms or fatigue – this was usually only after testing his posture limits, either sitting too long or bending over.
PROGNOSIS AND RESULTS:Mr H’s progress through the treatment plan has been challenging. Given the long and complex history Mr H presented with, the patient expectations were hopeful for achieving relief in the restrictions he felt in his active/ passive mobility and muscle imbalances. He welcomed and appreciated any improvements thus far. He attended regular appointments as instructed and was compliant with all investigative processes.
Mr H has shown decreased pain levels and improvements in functionality and range of motion (ROM) beyond 50%. He further reports less frequent and intense pain on occasion in the right flank/ hip region and slightly less tightness in the hamstrings intermittently. Mr H has slowly begun attempting to improve his physical fitness by sporadically bike riding and swimming. Occupational ergonomic instructions have resulted in improved workplace compliance with resulting physical benefits.
Mr H continues to attend fortnightly appointments while he continues to improve his physical strength and fitness. His treatment sessions still consist of Cox® Flexion-Distraction Protocol II (2) to the upper lumbar spinal levels and mobilization of the sacro-iliac joints. He maintains a steady 50% improvement on his initial presentation. We have progressed to include multiple regions of the spine, incorporating the cervicothoracic spine and further spinal muscular symmetry in conjunction with postural improvement strategies associated with his work environment.
CONCLUSION:Mr H’s long-term prognosis is guarded given the multi-level constraints and fixations in the lower lumbar spine; however, continued conservative management of his condition will ensure continued ease and physical ability for him to complete regular activities of daily living (ADLs) as well as alleviate continued joint irritation, progressive degeneration of the spinal levels above and below the fixated levels, and spinal nerve root compression.
Cox® Flexion- Distraction and Spinal Decompression Therapy has been useful at providing ongoing compartment mobility above and below the fused and degraded lower lumbar spinal levels. This is further demonstrated by the subjective and objective improvements that has been demonstrated and the ability for this patient to maintain a more active functional lifestyle.
REFERENCES:
- Cox JM, Feller J, Cox J. Distraction Chiropractic Adjusting: Clinical Application and Outcomes of 1000 cases. (1996).
- Low Back Pain: Mechanisms, Diagnosis and Treatment. James M Cox. 7th Ed. Lippincott, Williams & Wilkins. 2011.
- Gudavalli MR: Estimation of dimensional changes in the lumbar intervertebral foramen of lumbar spine during flexion distraction procedure. Proceedings of the 1994 International Conference on Spinal Manipulation, June 10‐11, 1994, Palm Springs, CA, pp 81.
- Gudavalli MR, Cox JM, Baker JA, Cramer GD, Patwardhan AG: Intervertebral Disc Pressure Changes During a Chiropractic Procedure. Proceedings of Bioengineering Conference, Phoenix, 1997
- Gudavalli MR, Olding, K, Joachim, G, Cox, J. Chiropractic Distraction Spinal Manipulation on Postsurgical Continued Low Back and Radicular Pain Patients: A Retrospective Case Series. J Chiropr Med. 2016 Jun;15(2):121-8. doi: 10.1016/j.jcm.2016.04.004. Epub 2016 May 25.



